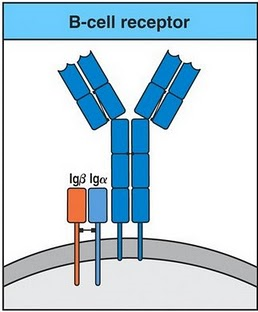
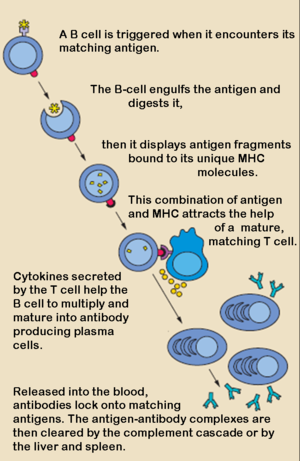
 The adaptive immune response is split into 2 pathways: the humoral response & the cell mediated response. The cells related to these pathways also vary: in the humoral response involves B lymphocytes (B cells), while the cell mediated response involves T lymphocytes (T cells). B cells are derived from the bone marrow and circulate through the blood stream, spleen and lymph nodes. B cells produce antibodies and each antibody is specific to that B cell. Antibodies can be in two forms: excreted (IgG, IgA) or expressed on the cell surface of the B cell (IgM, IgD). B cells also have receptors on the surface, this receptor along with the antibody form signalling complexes. The receptor is made up of two proteins: Igα & Igβ- antigen binds to Ig – Igα & Igβ initiate intracellular signalling events to activate B cells. T cells are produced in the thymus however precursor T cells are produced in the bone marrow and migrate to the thymus located in the mediastinum, once matured T cells will travel around the body. There are two types of T cells that derive from the thymus which can be distinguishable based on the molecules present on the cell surface. Helper T cells express a molecule called CD4 on their cell surface, therefore known as CD4 T cells (T helper cells). The other type of T cells express a molecule called CD8 on their cell surface, therefore known as CD8 T cells (known as cytotoxic after activation). CD4 & CD8 T cells use a receptor called T cell Receptor (TcR) to recognise antigens. The TcR is different to the antibody and the genes that code for it are on different chromosomes. The TcR is made up of two glycoprotein chains called α & β. Both chains have a similar structure to Ig, as the TcR has a variable and constant domain. TcR is always present on the surface of the T cells. Different T cells will recognise different antigens as each TcR will have different variable regions. T cells recognise antigens that are associated with molecules on the surface of cells called ‘major histocompatibility complex’ (HMC). MHC refers to a region of the DNA and is located on the chromosome 6 in humans. All vertebrate species have an HMC, and a unique name is given to it. In humans the MHC is called HLA (human leucocyte antigen). MHCs are split into 3 classes: class I, II & III. The CD4 &CD8 bind to the non-polymorphic region of the MCH to get stronger bonding. Once infected the first response will be dealt with B cells (primary response). All B cells differ from each other depending on the Ig variable region of the antibody. The antibody of the cell will bind to the antigen of the pathogen or foreign particle. Once activated, the B cell will undergo clonal selection (create the specific antibody), it will proliferate and differentiate into plasma B cells (effector cells) and B memory cells. The effector cells are involved in the phagocytosis of the pathogen. The B memory cells stay in the body and activate during the secondary response, if the same pathogen was to infect again. Once the B cell has ingested the pathogen it will go through antigen processing and presentation. Endogenous antigens are produced within the cell (viral proteins) and are processed and presented by Class I MHC. Exogenous antigens derive from outside the cell and are processed and expressed by Class II MHC molecules. All nucleated cells express class I MHC. Proteins are fragmented in the cytosol by proteosomes. The fragments are then transported across the membrane of the endoplasmic reticulum by transporter proteins. Synthesis and assembly of class I heavy chain and beta2 microglobulin occurs in the endoplasmic reticulum and transported to the cell surface. A limited group of cells express class II MHC, which includes the antigen presenting cells (APC). The principal APC are macrophages, dendritic cells, and B cells. The exogenous proteins are taken in by endocytosis are fragmented by proteases in an endosome. The alpha and beta chains of MHC class II are synthesized and assembled in the endoplasmic reticulum. Then transported through the Golgi to reach an endosome where the peptide fragments from the exogenous protein are transported to the cell surface. Infected cells present foreign antigen to CD8 T cells. The MHC Class I (antigen) is recognised by TcR (CD8 T cell). This activates the CD8 T cell; it then proliferates and differentiates to cytotoxic T lymphocyte (CTL). The CTL produces cytoplasmic granules containing enzymes (granzymes) and perforin. The CTL releases perforin that makes holes in the plasma membrane of target cell, the granzymes enter the target cell (via perforin pores) and triggers aptosis of the target cell. CD 4 T cells specialise in antigen presenting cells (APC) present antigen to CD4 T cell. The MHC Class II (antigen) is recognised by TCR (CD4 cell) but this does not activate the CD4 T cell yet. Another signal is required which is the interaction of CD80/CD86 on APC with CD28 on T cells. Once activated the CD4 T cells synthesises and secretes cytokine (interleukin 2 (IL2)) and expresses receptors for IL2. The IL2 causes proliferation of activated CD4 T cells and differentiation of CD4 T cells into either Th 1 or Th2. Th1 help macrophages and B cells, Th2 help B cells. Th1 secrete IFNγ, this IFNγ activates macrophages that increase expression of MHCII and increase antigen presentation to CD4 T cells activating more CD4 T cells. The overall effect of this will be the amplification of the immune response.
0 Comments
Leave a Reply. |
Details
This project began as a facebook page sharing information about different illnesses, diagnosis and treatments. We are now doing short articles :)
Health stuffArchives
April 2020
Categories |
 RSS Feed
RSS Feed