|
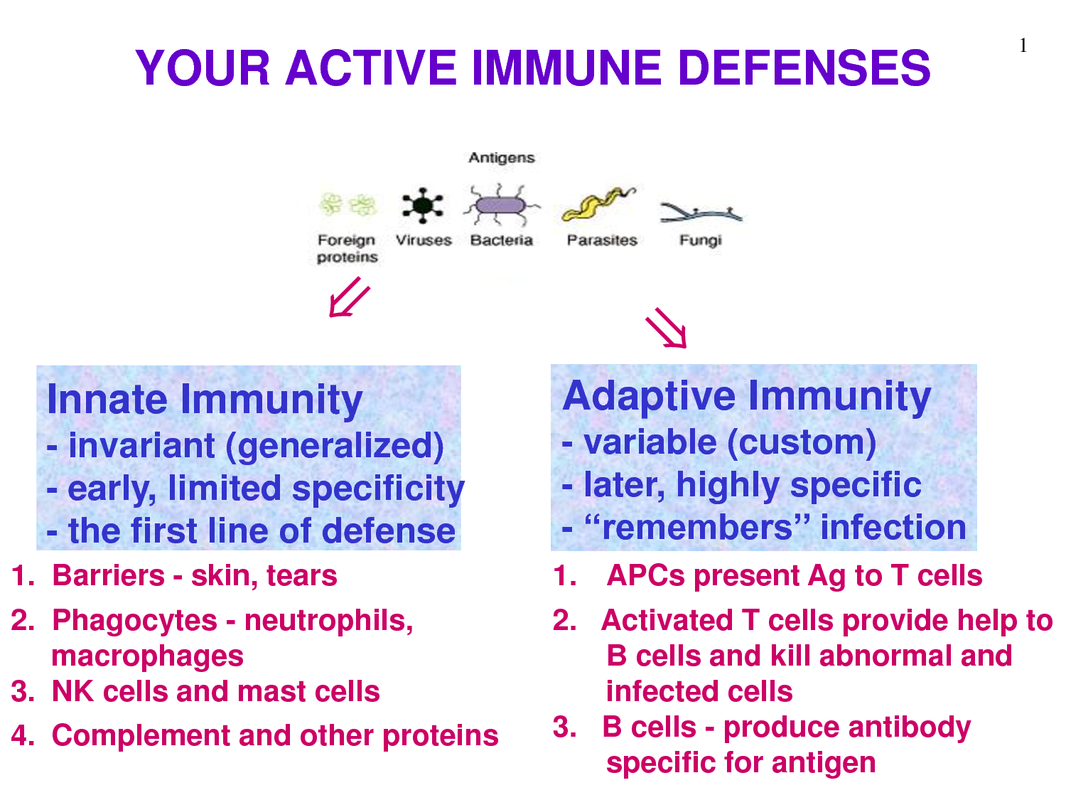
The immune system is the body’s way of fighting off invading pathogens. The immune system is composed of two parts: the innate immune response & the adaptive immune response. It is called the innate immune response as it is the pre-existing defence mechanisms that help prevent infection by pathogens or to create defence against an infectious agent. ‘Innate’ because it is present before an infection is occurs. The innate response in non-specific (whatever the pathogen: the response is always the same). It can be defined as the body’s first line of defence against pathogens. The physical, chemical & biochemical barriers are part of the innate response.
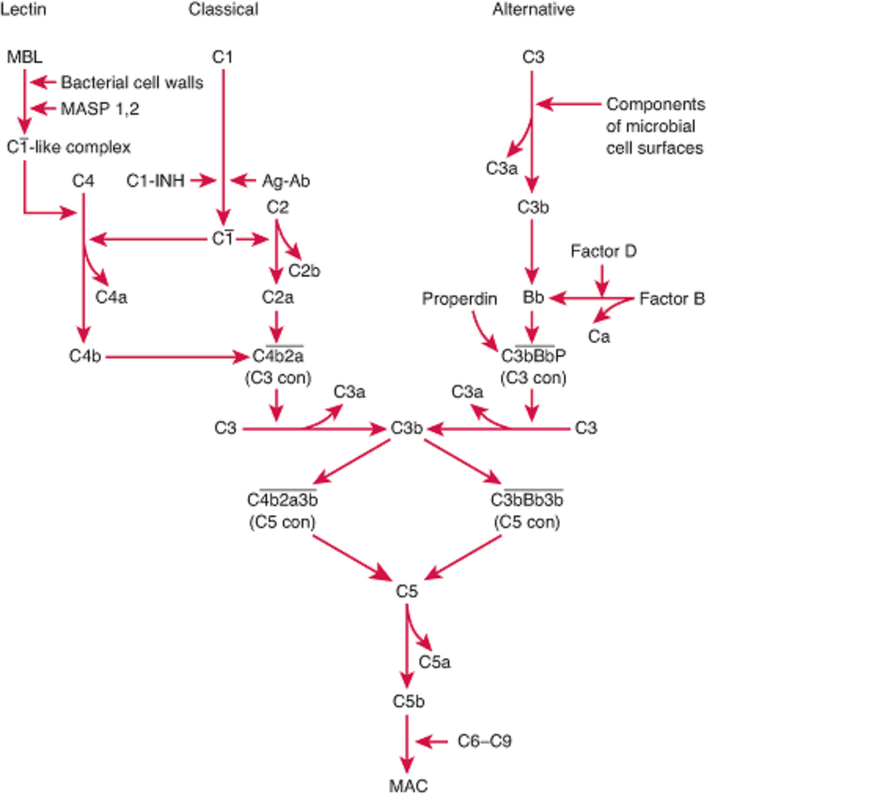
It is divided into 5 stages: (1) Awareness of the infection (2) Immediate response to the infection (3) Delayed response (if immediate is not effective) (4) Elimination of pathogen (5) Provision of immunity Many cells and proteins in the body are part of the innate immune system. They provide two functions: 1) they are able to recognise the presence of invasion 2) provide immediate cellular response. One of the main types of cell involved is macrophages: these are created in the bone marrow and are found in most tissues. Another is neutrophils, which can also leave the blood stream and enter damaged or infected tissue. Mast cells and dendric cells are also involved. Cells related to the innate response have receptors that recognise pathogens based on their characteristics. One type of receptor is called ‘mannose receptor’, which is a C-type lectin carbohydrate binding protein that recognises complex carbohydrates. CD-14 is another type of receptor that acts as a Co-receptor with TLR4 (toll like receptor) in detecting bacterial liposaccharides. TLR are a family of receptors that recognise a variety of pathogens (TLR1 – bacterial lipopeptide, TLR2 – peptidoglycan, TLR3 – dsDNA). Recognition is only useful if it helps in the elimination of the pathogen or if it limits its replication. The response once recognition is achieved is phagocytosis. Phagocytosis is the ingestion and destruction of the microbe. Phagocytosis is done by macrophages & neutrophils. Phagocytosis is split into four steps: attachment of the phagocyte to the particle to be phagocytosed, ingestion : by extending the membranes around the particle and engulfing it taking it into a vacuole, then killing the phagocyte and degrading it by using the enzymes present in the vacuole. Instead of phagocytosis, another process that can occur is the secretion of proteins known as cytokines, which are produced in response to pathogen stimuli. Sometimes there are not enough macrophages present to eliminate the pathogen, so additional phagocytes are called that have a variety of proteins. This response is known as the inflammatory response. Leukocytes have a unique ability to move around the body, in & out of blood vessels & tissues. The control of where these cells go is very important and is achieved by adhesion molecules & chemotactic agents. Adhesion molecules bind to each other in a specific manner and enable cells to interact with each other. Adhesion molecules include: glycoproteins (lectins –super binding molecules that can be expressed on leukocyte or endothelial cells) & Integrins (hetrodimeric proteins consisting of alpha & Beta chains that are expressed on the leukocytes). Extravasation is the process of cells leaving the bloodstream, crossing the endothelium layer and entering the tissue. This is split into 3 stages: (1) Rolling neutrophils: normally travel in the centre of the blood stream away from the endothelium. Once inflammation occurs, it will cause vasodilation disturbing blood flow causing the neutrophils to bump along the endothelium (rolling motion). Inflammatory mediators such as TNF-α, the endothelial cells are activated to express P-selectins & E-selectins on their surface. These selectins bind to sialyl-Lewisx on the surface of the neutrophil slowing it down and making it roll along the endothelium. (2) Activation and Firm attachment: the binding of the sialyl-Lewisx is not strong enough for the neutrophil to adhere to the endothelium. To achieve a strong attachment, a LFA-1 integrin on the neutrophil binds to the ICAM-1 on the endothelium. Before the LFA-1 can bind, it has to go through a conformational change. To do this it must bind to IL-8 (interleukin). IL-8 is a chemokine and produced in response to an inflammation. Some of the IL-8 are in the extracellular matrix on the endothelial surface and can bind to IL-8 receptors present on the neutrophil surface. Once conformation has occurred, LFA-1 can firmly bind to ICAM-1 on the endothelium. (3) Transendothelial migration: Once the neutrophil is attached to the endothelium, it squeezes between the endothelial cells making contact with the basement membrane and releases enzymes that digest away the membrane allowing the leukocyte to enter into the tissue. Complement system is made up of a number of plasma proteins that play a role in resistance to infection. It consists of pro-enzymes and other factors that activate each other in order to produce a variety of active proteins. The proteins involved are called C1-C9. Different complement pathways exist: classical, lectin & alternative. All pathways start off differently but have a common end stage. The end product is to form a MAC (membrane Attack Complex). This is the generation of a pore in the membrane that will result in the lysis of the cell. The pores allow ions and small molecules through, but not proteins. There is an influx of water into the cell leading to the lysis ‘bursting’ of the cell.
0 Comments
Leave a Reply. |
Details
This project began as a facebook page sharing information about different illnesses, diagnosis and treatments. We are now doing short articles :)
Health stuffArchives
April 2020
Categories |
 RSS Feed
RSS Feed